Focal Segmental Glomerulosclerosis (FSGS)
Contents
What is FSGS?
FSGS stands for Focal Segmental Glomerulosclerosis. It is a relatively common form of kidney disease, especially in the US. Although there are several known risk factors, we don’t yet know why most people develop FSGS. In order to be diagnosed with FSGS, you must undergo a kidney biopsy.
FSGS is named for the scarring, or “sclerosis,” that can be found in the kidney of people with this disease. When looked at under a microscope, everyone’s kidneys contain millions of tiny filters called “glomeruli”. These filters work much like a colander that you might have in your kitchen. Blood is “poured into them” as it circulates through the kidney, and the water-like part of the blood drains through. This becomes your urine. When these filters are damaged they become scarred. They are no longer able to filter blood appropriately. This is called “glomerulosclerosis”.
The word “focal” is added because in FSGS, only some of the filters are damaged. “Segmental” is included because often only parts of the filters are scarred.
So Focal Segmental Glomerulosclerosis is a very descriptive name for the disease. Some segments of kidney filters are scarred.
What does it look like?
First, a quick look at the kidney. Most people have two kidneys, one on each side of their lower back. All of the blood in your body passes through your kidneys many times during the day. Each time blood goes through some of it gets cleaned and filtered by the glomeruli (just one= glomerulus). This cleaning is how your body gets impurities out of the blood (and removes extra water). Some of the cleaned blood becomes your urine. Urine isn’t red like blood because the red blood cells, which give blood its color, are too big to fit through the filters. A glomerulus is just a tiny bag of blood containers through which blood gets filtered, and all of the clean blood (urine) runs into tubes (ureters) which eventually lead to your bladder.
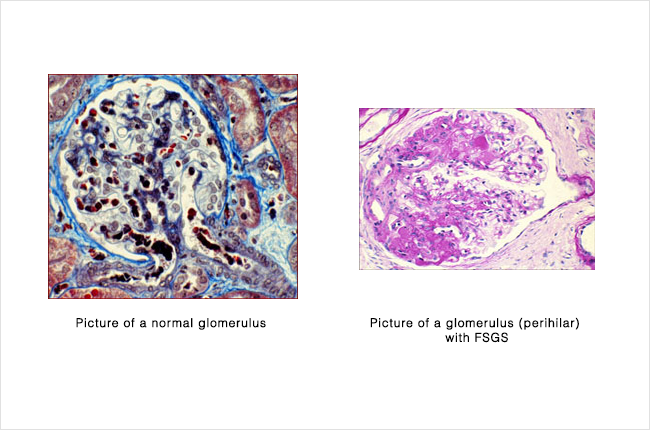
Above are shown two kidney filters, as they look under a microscope. On the left is a normal filter, and on the right is a filter from someone with FSGS. The right half of the filter with FSGS still looks a lot like the normal picture on the left. Again, that’s where the “Segmental” part of the name comes from. A healthy filter can be right next to a diseased filter. The left half of the picture on the right is scarred.
 |
 |
|---|
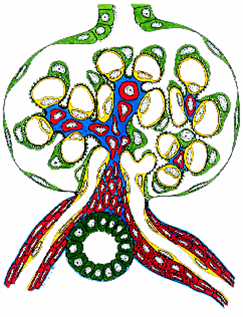
On left, graphic illustration of a normal glomerulus; on right graphic illustration of glomerulus with FSGS (perihilar)
Above are two more filters, this time shown as cross-sectioned drawings. Again, the normal filter is on the left. The red tubes at the bottom are where blood goes in and out. The green tube at the top is where urine exits. In between are all of the vessels that do the filtering (seen in yellow and green). Now look at the picture on the right. The bottom right of the filter has become nothing but scar (black). This portion of the glomerulus has become useless for filtering. It is also difficult for any blood to get through at all.
How did I get it?
The short answer is that no one is sure. Doctors tend to put FSGS in two big categories, primary and secondary. Primary means that the disease happens on its own, for no obvious reasons. Secondary means that we think the FSGS was caused by, or is associated with, another medical condition. How the other condition caused the FSGS scarring has not been completely figured out for all diseases. These are some of the secondary causes/associations.
- Kidney defects from birth
- Urine backing up into kidneys
- Obesity
- Obstructive Sleep Apnea
- Sickle Cell Anemia
- Viruses (such as HIV)
Most people with the above conditions do not have FSGS. Having FSGS does NOT put you at risk for any of these conditions you do not already have. However, having family members with FSGS does increase your chances of developing it yourself. Also, the disease is twice as common in blacks than in whites.
What are the symptoms?
Many people with FSGS have no symptoms at all. The most common complaint is edema, or swelling, especially in the legs. Often patients find that their shoes no longer fit, or that they have suddenly put on weight. High blood pressure, or hypertension, is also a very common finding. The hypertension in people with FSGS can often be very difficult to treat.
FSGS can also cause abnormal results in two different routine laboratory tests ordered by your doctor. The first is a test of kidney function called “creatinine.” It is measured by taking a blood sample. Everyone has a certain amount of a substance called creatinine floating in his or her blood. This substance is always being produced by healthy muscles, but since the kidneys constantly filter it out the level of creatinine stays low. When the filters become damaged, the level of creatinine left in the blood goes up. A higher level of creatinine alerts the doctor that the kidneys aren’t filtering as well as they should.
The second test is for protein in your urine. Urine normally contains only a very small amount of protein. It is just too big to pass through the filters. But when the filters become scarred or damaged, they can “leak” protein into the urine. If a doctor finds too much protein in your urine, it usually means something is wrong with the filters. Some people with a large amount of protein in their urine say that their urine looks “foamy,” like bubbles built up in dishwater.
None of the above symptoms, or even all of them together, is specific for FSGS. If you or your doctor are concerned about FSGS, the only way to know for sure is to have a kidney biopsy.
Biopsy Results
FSGS can have several different appearances, or variants, when seen under the microscope. There is still some debate between doctors about the importance of separating FSGS into these different variants. However, these different appearances can provide clues about what caused the disease or how it will behave. Below are the recognized variants. A representative drawing is on the left. An actual picture taken through a microscope is on the right. Compare these to the normal filter pictured above.
Tip Variant
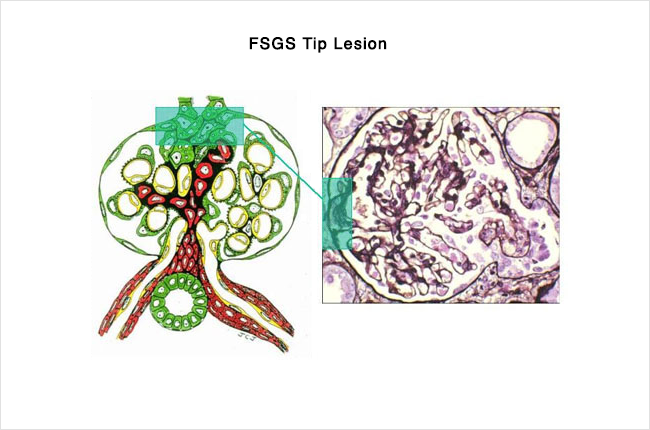
In the tip variant, the glomerular scarring and damage occurs at the “tip” of the filter. This “tip” is the beginning of the tube that carries away the urine, and it is usually on the opposite side of the filter from where the blood vessels enter and exit. In the picture on the left, the tip is at the top- you can see that the green tube exiting the top of the filter is blocked with a scar. The symptoms of FSGS in the tip variant often appear suddenly. There is a large amount of protein in the urine and a tendency to develop the full Nephrotic Syndrome (see below). This variant also seems to be the most responsive to treatment, with most of the patients who receive steroids undergoing a full or partial remission.
Perihilar Variant
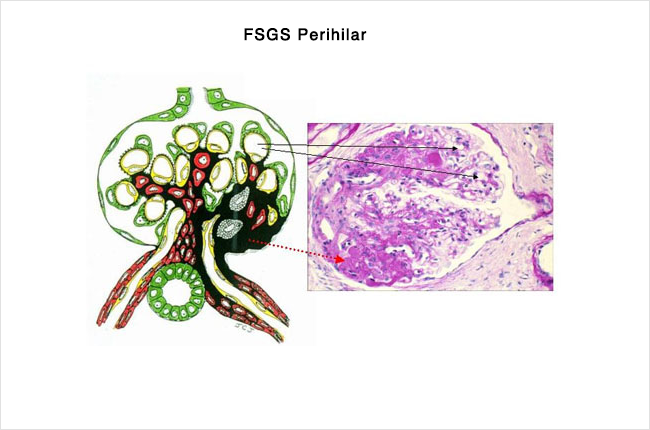
The perihilar variant has scar that forms at the hilum of the filter. This is where the blood vessels enter and exit. The hilumis at the bottom of the filter in the picture on the left. In this variant, the cause of the FSGS is often something that has previously caused a reduction in the number of filters someone has. Being born with only one kidney or having significant kidney damage early in life from reflux nephropathy can cause this type of damage.
Collapsing Variant
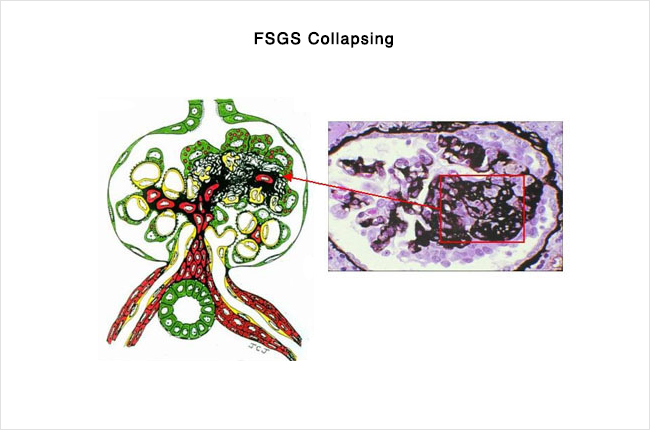
The collapsing variant is considered the most rapidly progressive form of FSGS. It does not typically respond to therapy. The scarring quickly affects the entire filter, causing it to collapse. Most patients that are diagnosed with the Collapsing variant will require dialysis or a kidney transplant within one to two years despite treatment. This variant was previously thought only to effect people with HIV. It is now found in increasing numbers of HIV-negative patients. Collapsing FSGShas also been associated certain drugs, such as pamidronate.
Cellular Variant
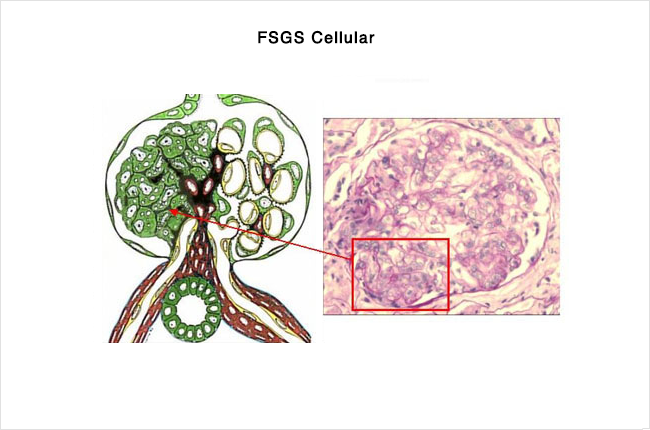
The cellular variant implies a slightly different type of scarring. The problem is an overabundance of cells that make up the filter itself. As these cells build up, the blood vessels that make up the filter narrow and eventually close off completely. This variant can only be diagnosed if none of the above variants are seen on the biopsy.

Classic FSGS
If none of the above specific variations are seen on biopsy, the disease is called Classic FSGS, or FSGS NOS. This stands for “not otherwise specified”. This form is generally less severe than the collapsing form. But having a diagnosis of Classic FSGS does not indicate how severe the disease will be, or how it will respond to treatment.
The Nephrotic Syndrome
FSGS is one of many diseases that can cause something called the “Nephrotic Syndrome.” When someone has a great deal of protein in their urine, they often develop a specific set of symptoms. The symptoms of the Nephrotic Syndrome always include-
- >3 g proteinuria (protein in the urine) per day
- Less protein in the blood than normal
- Swelling
It often also causes
- High cholesterol
- Increased tendency to form blood clots
What are my options for treatment?
FSGS is not an easy disease to treat. Anyone with this disease should be seen regularly by a kidney specialist, also called a nephrologist. If it is associated with any of the illnesses mentioned above, treating that particular illness becomes a priority. It is also important for someone with either primary OR secondary FSGS to be on medication that reduces the amount of protein in the urine. These medications are called ACE-inhibitors (angiotensin converting enzyme inhibitors) and ARBs (angiotensin II receptor blockers). If urine protein levels are high, the complications of the Nephrotic Syndrome should also be considered. Patients should receive routine cholesterol screening/treatment. Their physicians should always remember their tendency to form clots.
Finally, every patient with FSGS should have their kidney function monitored regularly with both blood and urine studies. As kidney function declines, certain other interventions may become necessary. No one’s kidney disease is exactly the same. Your nephrologist can tell you how often your labs need to be checked and what to expect if your kidney function begins to decline.
In addition to the above, many different types of drugs that suppress the immune system are also being used to treat FSGS. The most common of these are steroids. Unfortunately, all of these drugs have significant side effects. Their use must be considered on a patient-by-patient basis.
What are my chances of getting better?
If not treated, most patients with FSGS will eventually develop complete renal failure and require dialysis or a kidney transplant to survive. Even with treatment, many patients will still eventually require dialysis. How long this will take varies widely (2-20 years), and is difficult to predict. The appearance of your kidney biopsy under the microscope may give your doctor some idea of the time frame. Specific forms of FSGS have been associated with different rates of progression and responsiveness to therapy.
Kidney Transplant in FSGS
Unfortunately, many patients diagnosed with FSGS will eventually progress to kidney failure. Kidney transplant is a treatment option for these patients. Read more general information about kidney transplant here.
The risk of FSGS returning in the transplanted kidney varies from 20-50%. There are several risk factors that put patients at higher risk of recurrence of FSGS. They are:
- young age (< 15 years old)
- if it took you less than 3 years from the time the FSGS was found in your original kidneys to reach kidney failure
- the appearance of certain cells on your original kidney biopsy (your nephrologist would have that information)
- Caucasian (White) race
- if you lost a previous kidney transplant to a return of FSGS
Usually a return of FSGS in the transplant occurs very soon after the surgery. The FSGS can return within hours to days. Most episodes will be within the first year after transplant.
Is there any treatment for FSGS that comes back in a transplant?
The way that FSGS causes damage to the transplanted kidney is not entirely clear. There is some evidence that it may be due to a substance present in the blood. For this reason, some episodes of recurrent FSGS are treated with a procedure called Plasmapheresis. This procedure takes blood out of the body in small volumes. The damaging substance from the blood are removed. The rest of the blood is then returned to the patient. This therapy is most effective if started very soon after abnormal protein is detected in the urine.
In addition to Plasmapheresis, use of immunosuppressive medications (different than those used to prevent rejection of the kidney) is sometimes effective. Additionally, the use of medications to control blood pressure and reduce the protein in the urine is helpful.
Unfortunately, none of these treatments are very successful at treating FSGS that returns in the transplant.
If the FSGS does come back, will it cause me to lose my kidney transplant?
Over half of the patients with recurrent FSGS in their transplant will lose their kidney within 5 years. Of all the patients with FSGS who get a kidney transplant, about 15% will lose the kidney due to recurrent FSGS.