MPGN
Contents
What is MPGN?
Membranoproliferative glomerulonephritis (MPGN) is a disease that affects the glomeruli, or filters, of the kidneys. Most instances of MPGN are caused by other diseases or disorders, including autoimmune diseases (such as systemic lupus erythematosis), chronic infections (like hepatitis B or more commonly hepatitis C), monoclonal immunoglobulin deposition diseases, and hereditary diseases. However, a few cases are idiopathic, or of unknown cause. The idiopathic type of MPGN is seen more commonly in persons aged 8-30.
What does it look like (under the microscope)?
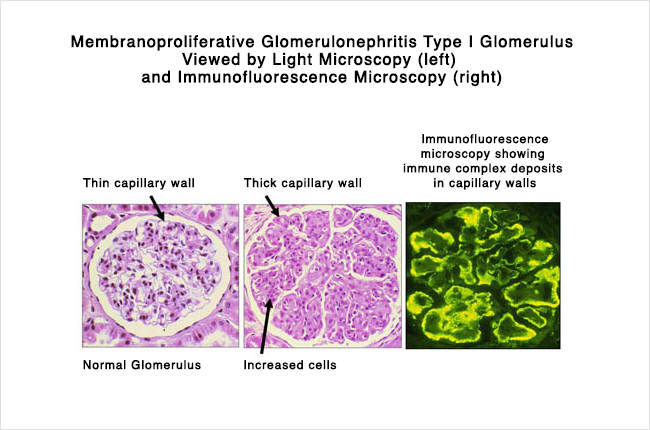
There are three histologic (microscopic) types of MPGN, each of which has a different appearance under the microscope.
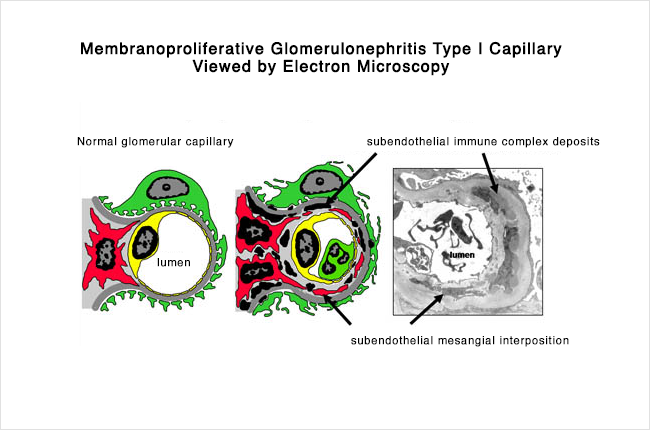
Type I – Discrete immune complexes are found in the mesangium and subendothelial space. Immune complexes are combinations of antigens and antibodies which bind to each other and then become lodged in the kidney. This activates the immune system, which causes inflammation and damage to the kidney itself.
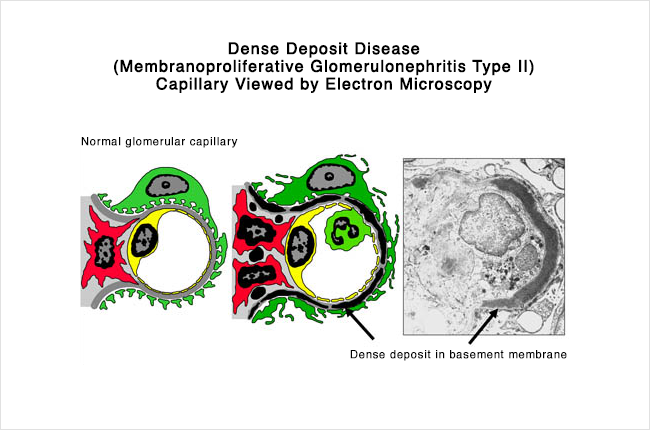
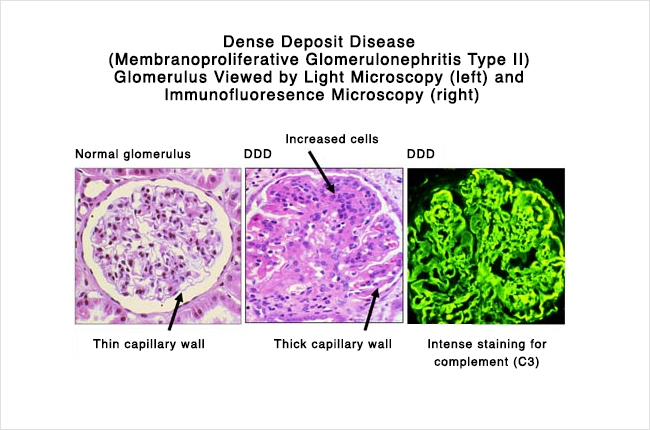
Type II – This is also called dense deposit disease. When viewed under the microscope, continuous, dense ribbon-like deposits are found along the basement membranes of the glomeruli, tubules, and Bowman’s capsule.
Type III – This is also an immune complex disease, similar to Type I. However, the immune complexes are found in the subepithelial space, and there is disruption of the glomerular basement membrane with large open areas.
How did I get it?
As stated above, MPGN is usually found in patients who have other diseases. The diseases associated most often are:
- Autoimmune diseases (most often systemic lupus erythematosus)
- Hepatitis B infection
- Hepatitis C infection
- Cryoglobulinemia
- Monoclonal immunoglobulin deposition diseases (such as AL amyloidosis and light and heavy chain deposition diseases)
- Subacute bacterial endocarditis
- Infection of a ventriculoatrial shunt
- Chronic lymphocytic leukemia (CLL)
So, if a patient is diagnosed with MPGN, the above associated diseases should be tested for and ruled out before the MPGN is considered idiopathic (of unknown cause). Also, as noted above, the idiopathic type of MPGN is seen more commonly in persons aged 8-30.
What are the symptoms?
The symptoms of MPGN are very similar to those of a focal glomerulonephritis. Specifically, patients have hematuria (blood in the urine), either macroscopic, which can be seen by the naked eye, or microscopic. Many of the red blood cells are dysmorphic (malformed or misshapen). In addition, mild or severe proteinuria can be found (including the nephrotic syndrome).
What is the treatment?
When MPGN is associated with another condition or disease, like any of the ones listed above, it is usually resolved by successfully treating the associated condition or disease. However, the optimal treatment of idiopathic MPGN is not entirely known.
The type of treatment will depend on the type of proteinuria that the patient has. If a patient has proteinuria that is “non-nephrotic”, then specific immunosuppressive therapy may not be necessary, as the long-term outcome is not life-threatening. However, patients with nephrotic-range proteinuria will typically be treated with steroids (Prednisone).
There are some treatments that patients try if the disease does not respond to steroids, including a trial of aspirin and dipyridamole, or a combination of cyclosporine and prednisone. However, the clinical trials that have been done on these types of alternative treatments have given us very limited data. Decisions regarding treatment should be made after significant discussion between a patient and his or her nephrologist.
What is the prognosis?
When MPGN is associated with another condition or disease, like any of the ones listed above, it is usually resolved by successfully treating the associated condition or disease. For example, if MPGN is associated with Hepatitis B or C viral infection, then MPGN tends to resolve either spontaneously or following treatment of the virus. Specific immunosuppressive therapy for MPGN is not necessary in this case.
Alternatively, if the MGPN is considered idiopathic, then the outcome is not as good. Up to 50-60% of untreated patients will progress to end-stage kidney disease within 10-15 years, while 25-40% of untreated patients will continue to have normal renal function. Spontaneous remission or improvement occurs in less than 10% of cases.
Patients with the following signs when they are first diagnosed have a worse prognosis:
- Nephrotic syndrome
- Kidney insufficiency
- Hypertension
- Crescents on kidney biopsy
However, even some of the patients with the above signs at the time of diagnosis can undergo a spontaneous remission.